

Vascular Diseases
Most people are familiar with heart disease and with the consequences of blockages in the blood vessels that carry blood to and from the heart. But few people realize that blockages caused by a buildup of plaque and cholesterol affect more than coronary arteries. Arteries throughout the body carry oxygen-rich blood away from the heart, so blockages can occur in all arteries with serious effects. Three of the most recognized vascular diseases include:
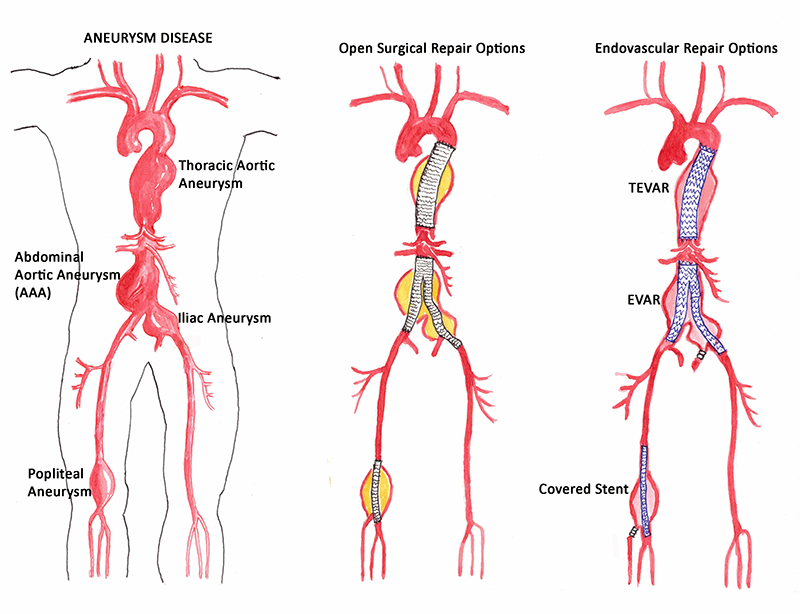
Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm (AAA) is an enlargement or “bulge” that develops in a weakened area within the largest artery in the abdomen. The pressure generated by each heartbeat pushes against the weakened aortic wall, causing the aneurysm to enlarge. If the AAA remains undetected, the aortic wall continues to weaken and the aneurysm continues to grow. Eventually, the aneurysm becomes so large, and its wall so weak, that rupture occurs. When this happens there is massive internal bleeding, a situation that is usually fatal. The only way to break this cycle is to find the AAA before it ruptures and to treat it surgically.


Carotid Artery Disease – Stroke
Carotid artery disease occurs when the main blood vessels to the brain develop a buildup of plaque caused by atherosclerosis, or hardening of the arteries. When the buildup becomes very severe, it can cause a stroke. A stroke occurs when part of the brain is damaged by these vascular problems; in fact, 80 percent of strokes are “ischemic strokes” where part of the circulation to the brain is cut off, usually due to blockages in the carotid arteries. The process is similar to the buildup of plaque in arteries in the heart that causes heart attacks. Strokes are the third leading cause of death in the United States according to the National Center for Health Statistics.
Peripheral Arterial Disease
Peripheral arterial disease (PAD) occurs when atherosclerosis, or hardening of the arteries, causes a buildup of plaque in the blood vessels that carry oxygen and nutrients to all the tissues of the body. As these plaques worsen, they reduce essential blood flow to the limbs and can even cause complete blockages of the arteries. Early PAD may only cause difficulty walking, but in its most severe forms, it can cause painful foot ulcers, infections, and even gangrene, which can result in major limb amputation. People with PAD are three times more likely to die of heart attacks or strokes than those without PAD.



Chronic Venous Insufficiency
Chronic venous insufficiency (CVI) is a condition that occurs when the venous wall and/or valves in the leg veins are not working effectively, making it difficult for blood to return to the heart from the legs. CVI causes blood to “pool” or collect in these veins, and this pooling is called stasis. Veins return blood to the heart from all the body’s organs. To reach the heart, the blood needs to flow upward from the veins in the legs. Calf muscles and the muscles in the feet need to contract with each step to squeeze the veins and push the blood upward. To keep the blood flowing up, and not back down, the veins contain one-way valves.
Chronic venous insufficiency occurs when these valves become damaged, allowing the blood to leak backward. Valve damage may occur as the result of aging, extended sitting or standing or a combination of aging and reduced mobility. When the veins and valves are weakened to the point where it is difficult for the blood to flow up to the heart, blood pressure in the veins stays elevated for long periods of time, leading to CVI.
CVI most commonly occurs as the result of a blood clot in the deep veins of the legs, a disease known as deep vein thrombosis (DVT). CVI also results from pelvic tumors and vascular malformations, and sometimes occurs for unknown reasons. Failure of the valves in leg veins to hold blood against gravity leads to sluggish movement of blood out of the veins, resulting in swollen legs.
Chronic venous insufficiency that develops as a result of DVT is also known as post-thrombotic syndrome (PTS). As many as 30 percent of people with DVT will develop this problem within 10 years after diagnosis.
Who is affected by chronic venous insufficiency?
An estimated 40 percent of people in the United States have CVI. It occurs more frequently in people over age 50, and more often in women than in men.
What are the symptoms of chronic venous insufficiency?
The seriousness of CVI, along with the complexities of treatment, increase as the disease progresses. That’s why it is very important to see your doctor if you have any of the symptoms of CVI. The problem will not go away if you wait, and the earlier it is diagnosed and treated, the better your chances of preventing serious complications. Symptoms include:
- Swelling in the lower legs and ankles, especially after extended periods of standing
- Aching or tiredness in the legs
- Varicose veins and spider veins
- Leathery-looking skin on the legs
- Flaking or itching skin on the legs or feet (stasis eczema)
- Stasis ulcers (or venous stasis ulcers)
If CVI is not treated, the pressure and swelling increase until the tiniest blood vessels in the legs (capillaries) burst. When this happens, the overlying skin takes on a reddish-brown color and is very sensitive to being broken if bumped or scratched.
At the least, burst capillaries can cause local tissue inflammation and internal tissue damage. At worst, this leads to ulcers, open sores on the skin surface. These venous stasis ulcers can be difficult to heal and can become infected. When the infection is not controlled, it can spread to surrounding tissue, a condition known as cellulitis.
CVI is often associated with varicose veins, which are twisted, enlarged veins close to the surface of the skin. They can occur almost anywhere, but most commonly occur in the legs.
Varicose veins and spider veins
Varicose veins and spider veins often occur in the middle-aged and can be uncomfortable and unsightly. They are the result of a condition call chronic venous insufficiency (CVI). For more information, see section on Chronic Venous Insufficiency.
Vascular Diseases
Most people are familiar with heart disease and with the consequences of blockages in the blood vessels that carry blood to and from the heart. But few people realize that blockages caused by a buildup of plaque and cholesterol affect more than coronary arteries. Arteries throughout the body carry oxygen-rich blood away from the heart, so blockages can occur in all arteries with serious effects. Three of the most recognized vascular diseases include
Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm (AAA) is an enlargement or “bulge” that develops in a weakened area within the largest artery in the abdomen. The pressure generated by each heartbeat pushes against the weakened aortic wall, causing the aneurysm to enlarge. If the AAA remains undetected, the aortic wall continues to weaken and the aneurysm continues to grow. Eventually, the aneurysm becomes so large, and its wall so weak, that rupture occurs. When this happens there is massive internal bleeding, a situation that is usually fatal. The only way to break this cycle is to find the AAA before it ruptures and to treat it surgically.
Carotid Artery Disease – Stroke
Carotid artery disease occurs when the main blood vessels to the brain develop a buildup of plaque caused by atherosclerosis, or hardening of the arteries. When the buildup becomes very severe, it can cause a stroke. A stroke occurs when part of the brain is damaged by these vascular problems; in fact, 80 percent of strokes are “ischemic strokes” where part of the circulation to the brain is cut off, usually due to blockages in the carotid arteries. The process is similar to the buildup of plaque in arteries in the heart that causes heart attacks. Strokes are the third leading cause of death in the United States according to the National Center for Health Statistics.
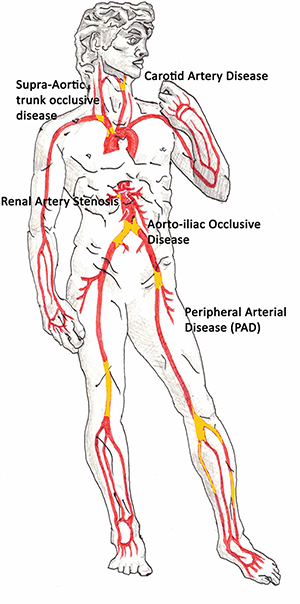
Peripheral Arterial Disease
Peripheral arterial disease (PAD) occurs when atherosclerosis, or hardening of the arteries, causes a buildup of plaque in the blood vessels that carry oxygen and nutrients to all the tissues of the body. As these plaques worsen, they reduce essential bloodflow to the limbs and can even cause complete blockages of the arteries. Early PAD may only cause difficulty walking, but in its most severe forms, it can cause painful foot ulcers, infections, and even gangrene, which can result in major limb amputation. People with PAD are three times more likely to die of heart attacks or strokes than those without PAD.
Chronic Venous Insufficiency
Chronic venous insufficiency (CVI) is a condition that occurs when the venous wall and/or valves in the leg veins are not working effectively, making it difficult for blood to return to the heart from the legs. CVI causes blood to “pool” or collect in these veins, and this pooling is called stasis. Veins return blood to the heart from all the body’s organs. To reach the heart, the blood needs to flow upward from the veins in the legs. Calf muscles and the muscles in the feet need to contract with each step to squeeze the veins and push the blood upward. To keep the blood flowing up, and not back down, the veins contain one-way valves.
Chronic venous insufficiency occurs when these valves become damaged, allowing the blood to leak backward. Valve damage may occur as the result of aging, extended sitting or standing or a combination of aging and reduced mobility. When the veins and valves are weakened to the point where it is difficult for the blood to flow up to the heart, blood pressure in the veins stays elevated for long periods of time, leading to CVI.
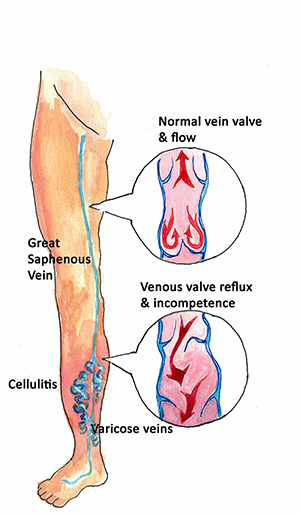
CVI most commonly occurs as the result of a blood clot in the deep veins of the legs, a disease known as deep vein thrombosis (DVT). CVI also results from pelvic tumors and vascular malformations, and sometimes occurs for unknown reasons. Failure of the valves in leg veins to hold blood against gravity leads to sluggish movement of blood out of the veins, resulting in swollen legs.
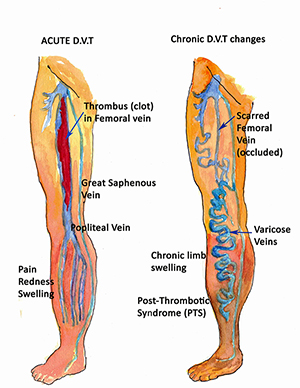
Chronic venous insufficiency that develops as a result of DVT is also known as post-thrombotic syndrome (PTS). As many as 30 percent of people with DVT will develop this problem within 10 years after diagnosis.
Who is affected by chronic venous insufficiency?
An estimated 40 percent of people in the United States have CVI. It occurs more frequently in people over age 50, and more often in women than in men.
What are the symptoms of chronic venous insufficiency?
The seriousness of CVI, along with the complexities of treatment, increase as the disease progresses. That’s why it is very important to see your doctor if you have any of the symptoms of CVI. The problem will not go away if you wait, and the earlier it is diagnosed and treated, the better your chances of preventing serious complications.Symptoms include:
- Swelling in the lower legs and ankles, especially after extended periods of standing
- Aching or tiredness in the legs
- Varicose veins and spider veins
- Leathery-looking skin on the legs
- Flaking or itching skin on the legs or feet (stasis eczema)
Stasis ulcers (or venous stasis ulcers)

If CVI is not treated, the pressure and swelling increase until the tiniest blood vessels in the legs (capillaries) burst. When this happens, the overlying skin takes on a reddish-brown color and is very sensitive to being broken if bumped or scratched.
At the least, burst capillaries can cause local tissue inflammation and internal tissue damage. At worst, this leads to ulcers, open sores on the skin surface. These venous stasis ulcers can be difficult to heal and can become infected. When the infection is not controlled, it can spread to surrounding tissue, a condition known as cellulitis.
CVI is often associated with varicose veins, which are twisted, enlarged veins close to the surface of the skin. They can occur almost anywhere, but most commonly occur in the legs.
Varicose veins and spider veins
Varicose veins and spider veins often occur in the middle-aged and can beuncomfortable and unsightly. They are the result of a condition call chronic venous insufficiency (CVI). For more information, see section on Chronic Venous Insufficiency.

